Ovarian reserve is a term that describes the number of healthy eggs a woman has left in her ovaries, which directly affects her ability to get pregnant.
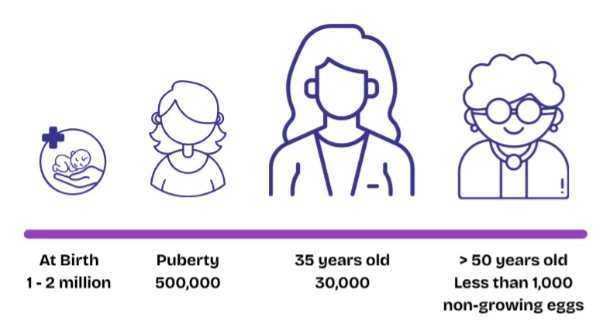
Women are born with a finite, non-renewable number of eggs that decline exponentially and irreversibly over time, leading to menopause when the egg supply is nearly exhausted. The initial reserve is usually around 1 to 2 million at birth, but this number steadily decreases as they age. By puberty, only about 500,000 eggs remain, and throughout a woman’s reproductive life, only a few hundred eggs will mature and be released during ovulation. The rest gradually die off naturally, and this natural decline continues until menopause (usually after 50 years old) when the ovaries no longer release eggs and menstruation stops.
In contrast, men continuously produce new sperm from puberty through old age, although sperm quantity and quality gradually decline with age, particularly after 50. Despite this decline, men generally remain fertile longer than women, whereas female fertility is tightly linked to the diminishing ovarian reserve.
The Importance of Ovarian Reserve Assessment
Testing a woman’s ovarian reserve is important because it provides valuable insight into her fertility potential and how she might respond to fertility treatments such as IVF. These tests estimate the quantity of remaining eggs compared to other women of the same age, helping to identify if the ovarian reserve is diminished, which can affect the likelihood of pregnancy. While ovarian reserve tests do not predict the exact ability to conceive or the quality of eggs, they guide fertility healthcare specialists in making informed decisions about fertility management and treatment planning. This information is especially crucial for women who are delaying pregnancy, experiencing fertility issues, or considering assisted reproductive technologies, as it helps tailor interventions and set realistic expectations.
Ovarian reserve assessment commonly includes three key tests:
- Day 2 (or Day 3) Follicle Stimulating Hormone (FSH) level,
- Antral Follicle Count (AFC), and
- Anti-Müllerian Hormone (AMH) measurement.
The Day-2 (or Day-3) FSH Fertility Test
A day-2 (or sometimes day-3) FSH blood test measures the concentration of follicle-stimulating hormone in a woman’s blood early in her menstrual cycle. This timing is chosen because hormone levels are more stable and provide a reliable baseline during this phase.
FSH is a hormone released by the pituitary gland that encourages the ovaries to develop follicles, which contain eggs. When the number of healthy eggs decreases, the ovaries produce less estrogen, prompting the pituitary to increase FSH production to stimulate follicle growth.
Therefore, higher-than-normal FSH levels on Day-2 can indicate a reduced ovarian reserve, signaling potential challenges with fertility. This test is a standard part of fertility assessments to help understand a woman’s reproductive capacity.
The Antral Follicle Count (AFC)
Antral follicle count (AFC) is a diagnostic procedure that assesses a woman’s ovarian reserve by counting the small follicles visible in the ovaries at the beginning of the menstrual cycle, typically between days 2 and 5, via transvaginal ultrasound scan.
These tiny follicles, each containing an immature egg, serve as an indicator of the number of eggs that could potentially develop during the cycle. Using a transvaginal ultrasound, a healthcare provider identifies and counts follicles measuring approximately 2 to 10 millimeters in diameter. A higher number of antral follicles usually reflects a healthier ovarian reserve and a better chance of responding positively to fertility treatments. Conversely, a lower count may suggest a reduced egg supply and possible challenges with fertility. AFC is widely regarded as a valuable tool in fertility evaluations and is often used alongside hormone tests to provide a clearer picture of reproductive potential.
The Anti-Mullerian Hormone (AMH)

Anti-Müllerian Hormone (AMH) is a hormone produced by the small follicles in a woman’s ovaries and serves as a useful indicator of her ovarian reserve. Unlike other hormones involved in the menstrual cycle, AMH levels remain relatively constant throughout the cycle, allowing the test to be performed at any time. Measuring AMH provides insight into the number of remaining eggs and helps predict how the ovaries might respond to fertility treatments. Higher AMH levels generally suggest a greater quantity of eggs, while lower levels may indicate a diminished ovarian reserve. Because it offers a convenient and reliable assessment, AMH testing is commonly used alongside other evaluations to guide fertility planning and treatment decisions.
The below is an indicative AMH reference range by age in ng/mL, based on multiple sources:
- 18-24 years: 2.1 – 6.8 ng/mL
- 25-29 years: 1.7 – 7.6 ng/mL
- 30-34 years: 1.5 – 5.6 ng/mL
- 35-39 years: 0.7 – 5.2 ng/mL
- 40-44 years: 0.3 – 2.6 ng/mL
- 45 years and above: 0.0 – 1.1 ng/mL
These values reflect the natural decline of ovarian reserve with age, where higher AMH indicates a larger pool of remaining eggs and lower AMH suggests diminished ovarian reserve.
For a comprehensive and personalized fertility evaluation, KL Fertility Centre offers a wide range of advanced diagnostic tests and expert care tailored to your unique needs. Our experienced specialists are dedicated to supporting you every step of the way, providing compassionate guidance and cutting-edge treatments to help you achieve your dream of parenthood. Whether you are just beginning your fertility journey or exploring options after challenges, we are here to empower you with knowledge and care.
Take the first step toward building your family with confidence—schedule your consultation today to get started on this important path to parenthood.